Presentation at the training program at the Natural and Health Sciences Research Center, Princess Nourah University, held on 08 January 2025. By Professor Omar Hasan Kasule Sr. MB ChB (MUK), MPH (Harvard), DrPH (Harvard) , Chairman of the Research Ethics Committee, KAAUH
Objectives:
- Main objective:
- To learn about the key concepts of ethical conduct of research
- Sub-objectives:
- To understand informed consent in pediatrics, assent or dissent, and subject respect
- Managing conflict of interest: Industry funding/Confidentiality, truth, and accuracy in reporting results
- Plagiarism
- Steps in submitting to PNU REB
Contents:
- Define research priorities and purposes (5%)
- Explain research ethics codes: Nuremberg, Helsinki, GCP (5%)
- Define the 2 major ethical issues: consent & adverse events (5%)
- Define other ethical issues related to patient safety: confidentiality, conflict of interest, truth telling and disclosure, research validity, and plagiarism (5%)
- Discuss informed consent: elements and issues (10%)
- Discuss adverse events: reporting and avoidance (10%)
- Analyze and discuss practical case scenarios involving ethical issues (60%)
Prioritizing Human Research:
- The general order of priorities is:
- necessities, dharuraat,
- needs, hajiyaat,
- complimentary, mukamillaat,
- embellishments, tahsinaat,
- excesses, israfaat,
- wastage, tabdhiraat.
- Medical research is a necessity (dharuraat) for two reasons:
- Better therapies: more effective, alternative, cheaper, easier
- Better physicians intellectually alive, up-to-date knowledge, inquisitive learners.
Purposes of Human Experimentation:
- Purpose 1: preserving morality, hifdh al ddiin
- Purpose 2: protection of life, hifdh al nafs
- Purpose 3: protection of progeny, hifdh al nasl
- Purpose 4: protection of the mind, hifdh al aql
- Purpose 5: protection of wealth, hifdh al maal
RESEARCH ETHICS CODES:
- Nuremberg Trials of Nazi Doctors:
- The Nuremberg Code at the end of the trials:
The Nuremberg Code 1946:
- Voluntary Informed Consent
- No Random Or Unnecessary Experiments
- Animal Experiments first
- Knowledge Of Disease Natural History
- Avoiding Unnecessary Physical And Mental Suffering
- The Researchers Must Be Scientifically Qualified
- Subjects Can Withdraw At Any Time
- The Investigation Is Stopped If The Patient Is In Danger.
Declaration of Helsinki Document 1964:
Helsinki Declaration 1962, 1996:
- Generally Accepted Scientific Principles
- Risk-Benefit Assessment
- Subject Integrity And Welfare
- Full Disclosure
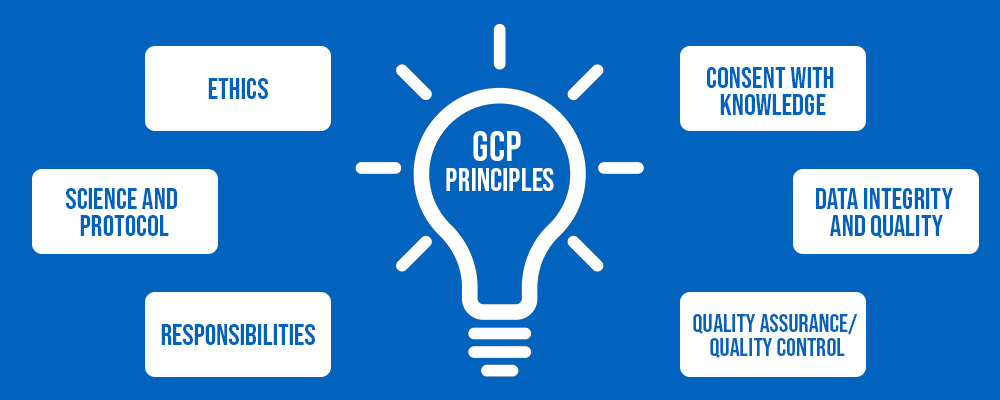
Good Clinical Practice Guidelines:
Good Clinical Practice Guidelines:
- Follow ethical principles of the Helsinki declaration
- Benefits justify risks
- Rights of patient > rights and interests of society
- Prior clinical and non-clinical information
- Follow protocol
- Qualified physicians
- Free informed consent
- Confidentiality
- Good manufacturing practice
- Quality control
Sections of the GCP Manual:
- The Institutional Review Board
- The investigator
- The sponsor
- Clinical trial protocol
- Investigator brochure
Good Manufacturing Practice Guidelines:
Saudi Ethics of Research on Living Creatures:
Major Ethical Issues in Research:
- Informed consent / autonomy:
- Frequently violated
- Autonomous right to protect life, hifdh al nafs
- Self interest in consent
- Competence to consent
- The benefit-risk ratio:
- The principle of injury, qa'idat al dharar
- Research policy aims at minimizing risk to research subjects
- Report and management of adverse events
INFORMED CONSENT:
Informed Consent Checklist (Required Elements):
- Participating, supporting, or organizing institutions and those who may benefit from the project’s results listed?
- A statement that the study involves research.
- An explanation of the purposes of the research.
- The expected duration of the participant’s participation.
- A description of the procedures to be followed.
- Identification of any procedures which are experimental (vs. standard care).
- A description of any reasonably foreseeable risks or discomforts to the participant.
- A description of any benefits to the participant or to others which may reasonably be expected from the research.
Informed Consent Checklist (Required Elements) con’t. - 1:
- A disclosure of appropriate alternative procedures or courses of treatment, if any, that might be advantageous to the participant.
- A statement describing the extent, if any, to which confidentiality of records identifying the participant will be maintained.
- If the research is subject to SFDA regulation, a statement that notes the possibility that SFDA may inspect the records.
- For research involving more than minimal risk, an explanation as to whether any compensation is available if injury occurs.
- An explanation as to whether any medical treatments are available if injury occurs.
Informed Consent Checklist (Required Elements) con’t. - 2:
- If so, what they consist of, or where further information may be obtained.
- An explanation of whom to contact for answers to pertinent questions about the research and research participants’ rights.
- Who to contact in the event of a research-related injury to the participant.
- A statement that participation is voluntary.
- A statement that refusal to participate will involve no penalty or loss of benefits to which the participant is otherwise entitled.
Informed Consent Checklist (Required Elements) con’t. - 3:
- A statement that the particular treatment or procedure may involve risks to the participant which are currently unforeseeable.
- The subject’s responsibilities.
- Any additional costs to the participant that may result from participation in the research.
- The anticipated prorated payment, if any, to the subject for participating in the trial.
- A statement that significant new findings developed during the course of the research which may relate to the participant’s willingness to continue participation will be provided to the participant.
Informed Consent Checklist (Required Elements) con’t. - 4:
- Anticipated circumstances under which the participant’s participation may be terminated by the investigator without regard to the participant’s consent.
- The approximate number of participants involved in the study (at this site and all sites).
Issues about consent:
- Competence and capacity in research
- Oral vs written/signed consent
- Payments in research
- Withdrawal of consent
- Research without consent
SAFETY OF RESEARCH SUBJECTS AND ADVERSE EVENTS REPORTING:
Three Main Categories of Research According to Risk:
- Exempt - no physical human risk. Approved immediately by the chairman and one or more members. Examples: interviews, questionnaires, information from records.
- Expedited - minimal human risk comparable to risk of routine outpatient procedures. Can be approved by the chairman with/without one or more members.
- Full review - major risk due to intervention on the human body either using drugs or devices. Approval follows discussion in a full meeting of the committee. The researchers may be invited to explain. Experts may also be consulted.
Discussion Cases on Risk-Benefit Considerations - 1:
- A resident refused to assist his consultant in a clinical trial on the grounds that from his personal experience the side effects of and reaction to the experimental drug were worse than the migraine headache. The consultant had a different view of the risk-benefit equation. The IRB had approved the study based on similar studies overseas with no reports of severe adverse reactions.
Discussion Cases on Risk-Benefit Considerations - 2:
- A systematic review of the literature showed that the proposed study had already been carried out in several countries and that the research question had been answered. The researchers still went ahead to submit the study to the IRB which approved it on the basis that the study had not been carried out locally.
Adverse events and protocol deviations / violations Datix reporting:
RESEARCH ETHICS BOARD / INSTITUTIONAL REVIEW BOARD (IRB):
The Institutional Review Board (IRB):
- Functions of IRB: assesses protocols that have ethical implications or has confidentiality issues, protect research subjects, protect researcher, protect the institution, monitor conduct of the research.
- Membership of IRB: professional and lay members.
- Procedures of IRB.
- Criteria of assessing research: Informed consent, clear objectives, sound research design, risks vs benefits, researcher qualifications, research facilities, data security.
- Follow-up of research: reports, onsite inspections, adverse event reports, protocol adherence.