Presentation at a “Clinical Research Course for Pediatric Residency Program” held via at Online King Fahad Medical City, Riyadh on 31 January 2021. By Professor Omar Hasan Kasule Sr. MB ChB (MUK). MPH (Harvard), DrPH (Harvard) Professor of Epidemiology, King Fahad Medical City
FUNCTIONS OF IRB
- Initial evaluation and approval of research proposals to make sure they fulfill the requirements of the Saudi regulations on human research and the international consensus Good Clinical Practice Guidelines. Above these regulations, IRB must ensure the highest ethical standards in any research.
-
Follow-up evaluation and approval of matters arising in the course of the research: protocol amendments, study termination/completion.
Monitoring of study execution by checking on vital issues such as proper consenting procedures, the confidentiality of the data, complete and up-to-date documentation, completeness and quality of AE reporting[1], and any ethical violations/protocol deviations.
MEMBERSHIP OF IRB - 1
- Membership of the IRB must have a diversity of medical professional competencies (clinical and non-clinical) to make sure that for every project reviewed there is a member from the relevant discipline and not necessarily the sub-discipline. Physicians tend to dominate IRBs.
- Membership should comprise representatives of the major medical and surgical specializations practiced in the hospital or region, hospital physicians, hospital nursing staff, general practitioners, pharmacists, statisticians, ethicists, and lay persons from the community.
- At least one of the members must be a normal community representative with no affiliation to the institution. This member should not have any connection with medical work.
MEMBERSHIP OF IRB - 2
- In selecting members attempts should be made to make sure that all genders and age groups are well represented.
- Members should be selected on their own personal merit as people with knowledge, skills, and sound judgment. They should discuss the proposals as individuals and not representatives of any department, unit, organization or profession.
- Members are appointed by the hospital, the health authority in the region or the government.
- The period of service on the committee is usually three years. Membership may be renewed. Staggered renewal of membership. A member should serve 2-3 terms.
SCOPE OF RESEARCH REVIEW BY IRB
- The committee assesses research proposals and protocols that have ethical implications: (a) research on patients, volunteers, the recently dead, fetal or embryological tissues (b) research with potential to breach confidentiality.
- All research however must be submitted to the IRB Chairman because the researcher cannot be trusted to determine the classification.
- The Chairman will determine which proposals are exempt (no risk no ethical issues) and which are expedited (minimal risk) and approve them immediately.
- The chairman will determine and approve expedited proposals (minimal patient risk) and if need be can consult one or more members of the committee.
- Full review is done for research with human intervention.
DOCUMENTS SUBMITTED FOR IRB REVIEW
- Exempt proposals submitted on a special form with the proposal attached. The form must be signed by the PI and HOD.
- Full and expedited: Protocols, investigator brochures, and consent documents of proposals with potentially significant patient risk are sent to all IRB members at least 2 weeks in advance for review with those from the relevant disciplines being asked to make a more detailed analysis and make a presentation to the IRB.
- The CVs of investigators and certification of GCP must be attached.
IRB MEETING
- The committee must be provided with adequate secretarial and logistic assistance to carry out its functions well.
- A quorum of at least half of the members will be necessary for holding a meeting. Members who cannot attend can send written comments and may/may not vote.
- The committee meets in private to preserve confidentiality. Others argue that they should meet in public for more transparency.[3]
- If the issues are complicated the investigator may be invited to the meeting to explain.
- Any member of the committee involved in a project will recluse himself when that project comes up for discussion.
CRITERIA OF IRB APPROVAL - 1
- The two main considerations in IRB decisions are: informed consent and patient safety.
- Informed and voluntary consent following full
disclosure of objectives, risks and benefits of the research, the right to
abstain or withdraw from the study. Special scrutiny of proxy consent for the
vulnerable will be made to ensure there is no abuse[4,5,6]. The
investigator must submit reasons in writing in cases in which full disclosure
is deemed inappropriate.
- Patient safety based on careful weighing of
benefits and risks.
- Confidentiality (use of certificates of
confidentiality7) and security of the data.
CRITERIA OF IRB APPROVAL - 2
- Scientific merit: objectives clearly states
and attainable, research design and statistical methods are adequate to produce
clinically and scientifically useful results. Outside experts may be
consulted. The committee will compare
the scientific merit and benefit of the research against risks and costs to
patients. Decision making procedures may improve the risk-benefit discourse[8].
- Qualification of the researchers based on study of
their detailed resumes.
- Adequacy of research facilities
- No conflicts of interest
EXEMPT - REQUEST REVIEW
EXPEDITED - REQUEST REVIEW
EXPEDITED - REQUEST REVIEW, con’t.
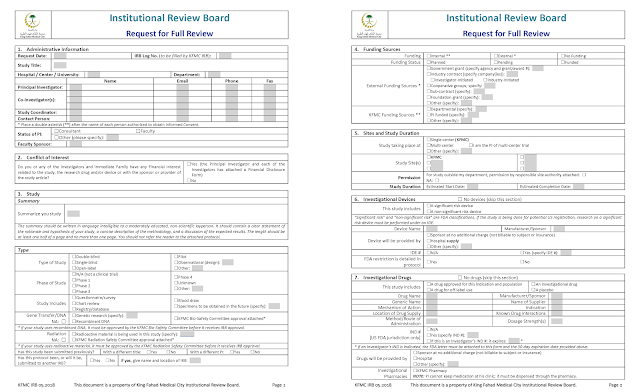
FULL - REQUEST REVIEW
FULL - REQUEST REVIEW, con’t. - 1
FULL - REQUEST REVIEW, con’t. - 2
EXEMPT CONSENT
EXPEDITED CONSENT
EXPEDITED CONSENT, con’t.
FULL REVIEW CONSENT, con’t. - 1
FULL REVIEW CONSENT, con’t. - 2
CASE REPORT CONSENT
AMENDMENT FORM
DECISIONS OF IRB
- IRB decisions are best taken by consensus but if this is not possible the decision will be based on a simple majority of the members attending if the quorum is assured. Minority views should be recorded.
- The decision of the committee may be full approval, conditional approval, deferment, or rejection. Reasons should be provided for projects approved conditionally or those that are rejected. If the investigator fulfills the missing information the chairman may approve a conditional approval without returning to the full committee.
FOLLOW-UP OF RESEARCH
- The committee must monitor progress of the research project and must receive reports of all adverse reactions whether related to the drug tested or not. AE reports from all sites of multi-center trials must be submitted.
- Members of the committee can make on-site inspections to make sure that the approved protocol is adhered to and to inspect research documents and records.
- Regular monitoring meetings are held to review the following: progress of recruitment of research subjects, changes to the protocol, adverse reactions, the process of informed consent, refusals and withdrawals, and case record forms.
- Warning letters.[9]
OVERSIGHT OF IRB
- The committee keeps full records of all its actions. Records are not privileged if a suit arises.
- It submits an annual report listing all proposals considered in the past year, the number approved, and any matters that deserve attention from higher authorities.
- The Chairman of IRB reports to the highest official in the institution.
- Tool for IRB self-assessment[10].
- Researchers have a right of appeal.
APPROVAL OF MANUSCRIPTS
- All manuscripts whether case reports or research require approval by IRB.
- It is against the law to submit to journals before IRB approval.
- Some journals insist on an IRB approval letter before accepting a manuscript.
- IRB checks the manuscripts to make sure they are from the approved research.
- IRB checks for ethical violations, data validity, authorship.
- IRB also checks for any statements against the culture and religion.
PROBLEMS OF IRB 1: HUMAN AND MATERIAL RESOURCES
- Not enough resources (financial, secretarial, office space) for their work.
- Chairman has a lot of administrative duties because of fulfilling research regulations and legal documents needed by international sponsors.
- Work of IRBs moving from ethics to research governance[11].
- IRBs struggle to catch up with new clinical research regulations[12].
PROBLEMS OF IRB 2: MEMBERS
- Members’ training needs often not fulfilled: lack of time & changing regulations. A specific curriculum is needed covering: committee working; scientific method; ethical analysis and the regulatory framework[13].
- Community member participation is limited[14]. Confusion about the roles of nonaffiliated and non-scientific members[15]. Varying ways of using community members[16].
- Conflicts of interest within IRB[17]: the obvious and the non-obvious.
IRB PROBLEMS: SUBMISSIONS - 1
- Poorly designed and written research proposals. Many procedural errors;[18] IRB normally gives researchers advice on improving their proposals instead of rejecting them outright.
- Sponsored research is over-documented and the sponsors expect IRB to review and approve many documents that have no direct relation to research ethics.
IRB PROBLEMS: SUBMISSIONS - 2
- What projects to review: Determination of minimal risk is not easy for example is trauma and sex survey minimal risk?[19] Is Medical education research under IRB review?[20,21] Are quality improvement projects research?[22] Chart reviews, case reports, observational studies part of IRB?[23] IRBs have problems dealing with community-based research.[24]
- Retrospective approvals to enable publications.
- Problem of dealing with incidental findings.[25]
IRB PROBLEMS: GUIDELINES - 1
- Inconsistencies among IRBs[26] and difficulty in setting standards[27]. No homogenous code, improper application of standards, lack of auditing capabilities[28].
- Different IRBs emphasize different criteria[29]. IRBs do not uniformly follow the common rule[30]. Common guidelines reduce variability[31].
IRB PROBLEMS: GUIDELINES - 2
- Varying decisions of IRBs for multicenter proposals[32,33,34,35,36,37]. Centralized IRBs have been suggested to standardize but they also have their problems[38,39]. Cost-benefit considerations[40]. Centralized IRBs are remote from researchers and the site of research? Wring decisions.
- Should IRBs follow centralized guidelines or should add their own local ones?[41] Should IRBs consider community values?[42]
IRB PROBLEMS: DIFFICULT DECISIONS - 1
- Problems in making decisions on re-use without informed consent that involves stored tissue[43] for the same research or different research.
- Deciding on research genetic research (confidentiality and sending material overseas. Researcher and IRB Chair perspective on genomic research were different[44].
IRB PROBLEMS: DIFFICULT DECISIONS - 2
- Hot protocols: facial transplants require different approaches[45].
- Issues of consent: Online survey tools may not fulfill consent rules[46]. Waiver of consent for emergency research[47], long consent forms / Arabic translations.
- Is IRB a rubberstamp function: Most research projects submitted are approved[48]. The majority of IRBs are satisfied with submissions by sponsors[49].
REFERENCES
- Clin Cancer Res. 2009 Jun 1;15(11):3850-5.
- BMC Med Ethics. 2010 Jun 28;11:12.
- J Med Ethics. 2008 Aug;34(8):631-5.
- Arch Dis Child. 2010 Nov;95(11):915-7.
- J Med Ethics. 2009 Jun;35(6):377-81.
- Crit Care Med. 2010 Nov;38(11):2146-54.
- PLoS One. 2012;7(9):e44050.
- BMC Med Ethics. 2012 Apr 20;13:6.
- Audits Indian J Med Ethics. 2011 Oct-Dec;8(4):211-4.
- J Empir Res Hum Res Ethics. 2010 Sep;5(3):85-96; quiz 97-8.
- MonashBioeth Rev. 2011 Sep;29(4):14.1-16.
- ClinDermatol. 2009 Jul-Aug;27(4):375-83.
- J Med Ethics. 2012 Mar;38(3):184-6.
- J Empir Res Hum Res Ethics. 2012 Feb;7(1):1-6.
- Acad Med. 2012 Jul;87(7):842-4.
- Acad Med. 2012 Jul;87(7):975-81.
- Acad Med. 2009 Apr;84(4):488-94.
- J Med Ethics. 2009 Feb;35(2):130-2.
- Psychol Sci. 2012 Jul 1;23(7):780-7.
- Acad Med. 2008 Jun;83(6):590-5.
- Acad Med. 2011 Jul;86(7):809-17.
- J Nurs Educ. 2013 Jan;52(1):51-5.
- Respir Care. 2008 Oct;53(10):1350-3.
- Environ Health. 2010 Jul 16;9:39.
- J Law Med Ethics. 2008 Summer;36(2):352-5, 213.
- Ger Med Sci. 2009 Jul 16;7:Doc07.
- J Med Ethics. 2009 Jun;35(6):382-3.
- Cent Eur J Public Health. 2012 Dec;20(4):297-8.
- Dev World Bioeth. 2008 Dec;8(3):207-18.
- Acad Med. 2012 Jul;87(7):969-74.
- Nurs Outlook. 2010 Jul-Aug;58(4):181-7.
- J Perinatol. 2010 Mar;30(3):163-9.
- Med Care. 2012 Jul;50 Suppl:S77-81.
- Ann Intern Med. 2012 May 15;156(10):728-35.
- Female Pelvic Med Reconstr Surg. 2012 Mar-Apr;18(2):89-92.
- J Healthc Qual. 2012 Jul-Aug;34(4):33-9.
- J Urol. 2009 Jun;181(6):2674-9.
- Acad Med. 2012 Dec;87(12):1710-4.
- Ann Neurol. 2010 Feb;67(2):258-60.
- J ClinOncol. 2010 Feb 1;28(4):662-6.
- J Am Board Fam Med. 2009 Jul-Aug;22(4):453-60.
- Med Law. 2010 Mar;29(1):37-50.
- J ClinPathol. 2009 Sep;62(9):825-9.
- Genet Test Mol Biomarkers. 2012 Jun;16(6):508-13.
- J Empir Res Hum Res Ethics. 2009 Jun;4(2):37-48.
- Am J Bioeth. 2010 Oct;10(10):5-8.
- J Med Ethics. 2008 May;34(5):393-5.
- Pharmacogenomics J. 2009 Apr;9(2):86-9.